Arthritis and arthritis are diseases characterized by pathological changes in the joints, however, the differences between arthritis and arthritis are significant. In order to understand the difference between arthritis and arthropathy, it is necessary to consider the etiology, pathogenesis, symptoms of arthritis and arthropathy. There are also different approaches to the treatment of joint disease and arthritis.
What is arthritis, joint disease? How do joint lesions of arthritis and arthropathy manifest, and what is the difference? In arthropathy and arthritis, the difference is due to the mechanism by which the pathological changes occur.
Arthropathy and arthritis treatment are long-term and multifactorial. Often, arthritis and arthropathy can be viewed as successive stages of the pathological process due to untimely treatment. Now that we understand what arthritis and arthritis are, we will determine the difference between arthritis and arthritis.
arthritis, classified
Arthritis - due to inflammatory changes, combined with the pathology of the joint itself, and is a symptom of other diseases, their failure. How arthritis is treated depends on identifying what is causing the inflammatory process.
According to the cause, there are:
- Primary - Rheumatoid, Rheumatoid Arthritis, Ankylosing Spondylitis, Still's Disease, etc.
- Secondary - complications of infectious, non-infectious processes (reactions with chlamydia, hepatitis, gastrointestinal disorders, septic lesions).
By number of affected joints:
- Monoarthritis - failure of a single joint.
- Polyarthritis - when a group of joints are affected.
Depending on the nature of the disease process:
- Acute arthritis - vivid clinical manifestations with inflammatory changes in the connective tissue of the joints.
- Subacute - an intermediate option, addressing the stage of an acute condition.
- Chronic arthritis - disappearance of clinical manifestations, slow course, with periods of decay and exacerbation.
Osteoarthritis, classified
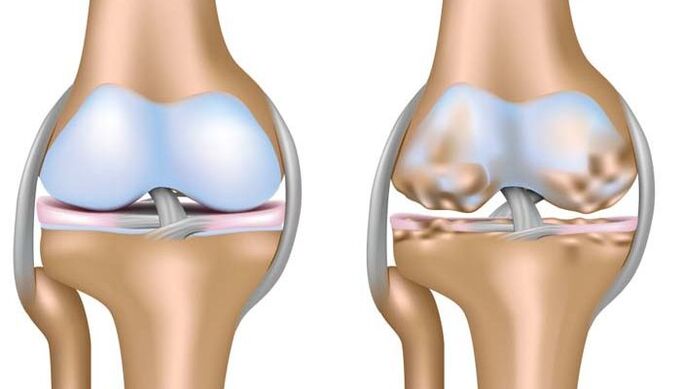
Osteoarthritis deforma, rheumatoid arthritis or arthropathy is a disease based on degenerative changes associated with the destruction of all joint structures, cartilage, ligaments, muscles, tendons and bones. This is the main difference between joint arthropathy and arthritis, resulting in irreversible deformity, dysfunction, and disability of the affected joint surface.
- Idiopathic - unknown cause. The pathological process is based on the autoimmune mechanism of the injury (primary rheumatoid arthropathy in young patients).
- Secondary osteoarthritis is the result of metabolic disturbances, trauma and inflammation. For example, rheumatoid arthritis that develops after suffering from rheumatoid arthritis.
arthritis, cause
Risk factors are:
- Violation of metabolic processes in the body.
- Genetic predisposition factors.
- Infectious diseases.
- Immunodeficiency state, presence of autoimmune diseases, allergic manifestations.
- Increased load on the musculoskeletal system due to professional activities and traumatic components.
joint disease, cause
Risk factors for developing osteoarthritis are:
- age. Osteoarthritis is a disease of the elderly, with the exception of rheumatoid arthritis, which occurs during adolescence. According to the World Health Organization, about 10% of the world's population suffers from joint disease.
- The body is overloaded, injured, and overweight, which increases the load on the joints. Large joints are more susceptible than others: hip-hip disease, knee-knee disease.
- Genetic factors: characterization of metabolic processes, cartilage tissue structure.
- The inflammatory process occurs without proper treatment.
arthritis, symptoms

Regardless of the cause of the disease, the signs of the disease have similar clinical manifestations during the acute phase of the process and during the exacerbation of the chronic course of the disease.
- Pain is the first symptom. It comes in varying intensities, is usually permanent, and does not depend on physical activity.
- Hyperemia of the skin in the joint area, increased local temperature (hot joint area), marked edema.
- There is an accumulation of fluid (fluid) in the joint pocket cavity. Microbiological and cytological examination of fluid from the inflamed cavity is important for diagnosis and can identify causative factors. The knee joint is more commonly affected. The presence of the inflammatory nature of the fluid within the joint capsule is the difference between arthritis and knee arthropathy.
- Extra-articular manifestations of the underlying disease: fever, vascular damage - vasculitis, heart valve, lung disease - alveolitis, pneumonia, kidney damage - nephritis, skin manifestations, hematological changes - anemia, increased platelet count in peripheral blood.
- Joint range of motion is limited, dysfunction.
osteoarthritis, symptoms

The symptoms of arthropathy are caused by long-term malnutrition and blood supply to the cartilage plate. Cartilage loses its elasticity and becomes thinner, while growths -- osteophytes -- form from the bony tissue within the joint cavity, irreversibly deforming the joint surface, disrupting function, causing pain, and significantly limiting mobility.
- pain. Attacks are characterized by moderate intensity, pain, and persistent pain. Enhancement of pain syndromes is associated with increased dystrophic changes in cartilage and deformity. Pain may vary and be temporary: it persists and subsides from morning stiffness through the day. A rapid, severe increase in pain is a sign of a poor prognosis.
- Deformation is visible.
- Dysfunction: flexion, extension.
- A characteristic creaking sound when moving.
- The development of joint immobility can lead to disability in the patient.
Osteochondrosis is a common spinal pathological condition caused by the same changes in cartilage as arthropathy.
diagnosis

The diagnosis of arthritis and arthropathy aims to determine the underlying cause of the disease, determine the activity of the process, assess the prognosis and effectiveness of treatment, and diagnose complications of the disease in a timely manner.
The comprehensive range of diagnostic tests includes general clinical laboratory tests, instrumental studies of the liver, kidneys, X-ray diagnostic measures, microscopy, and bacteriological studies.
- Distinctive features of arthritis of various etiologies are: increased erythrocyte sedimentation rate, increased levels of leukocytes in peripheral blood, which allow determination of the severity of inflammatory changes, increased plasma C-reactive protein - an important laboratory diagnostic test.
- X-rays allow you to see characteristic pictures of the surface of an inflamed joint.
- MRI is the most informative method for detecting inflammatory changes within the joint capsule.
- Use Doppler ultrasonography.
- In difficult cases, arthroscopy can be performed for differential diagnosis and treatment.
X-rays are an informative method that allows you to establish a diagnosis and differentiate between arthropathy or arthritis. Four degrees of pathological changes in arthropathy can be distinguished based on the identified changes, the degree of deformation of the cartilage in the joint, and the width of the joint space.
Arthritis, principles of treatment

Treatment of arthritis is long-term, with the main goal of curing the disease causing inflammatory changes in the joint capsule or achieving a long-term recurrence-free course, preventing the development of irreversible changes, deformities, and improving the quality and life expectancy of patients.
Widely used to treat:
- Affecting medical methods. Depending on the etiology, the following drugs are used: antibacterials, non-steroidal anti-inflammatory drugs, hormones, direct introduction of anti-inflammatory drugs into the joint cavity, in severe forms of rheumatic diseases, chemotherapy drugs are prescribed.
- non-drug treatment. Physical therapy exercise, adherence to diet, healthy lifestyle (smoking cessation, alcohol withdrawal, physical therapy, timely orthopaedic care and correction of existing conditions, prevention of progression of concomitant diseases) play an important role.
- Surgical methods are not the preferred method of treatment. This is a means of helping patients in particularly difficult situations - with the development of serious complications, severe pain syndromes, ineffectiveness of the first two treatments. It has certain signs of restrictions and appointments.
osteoarthritis, treatment

Comprehensive treatment for rheumatoid arthritis, including:
- non-drug treatment. In rheumatoid arthritis, treatment includes physical therapy exercises, physical therapy, protective regimens, load reduction, dieting, and weight loss.
- Medication is associated with pain relief. NSAIDs, hormonal drugs are more commonly prescribed.
- Surgical treatment methods: plastic surgery, arthrodesis, large joint (knee, hip) prosthesis.
prevent deterioration
Because the disease may have a long, chronic course, the development of complications, regardless of the cause of its occurrence, the patient needs to undergo continuous or long-term observation, and rehabilitation measures are designed taking into account the individual characteristics and nature of the disease.
Important preventive values are:
- Treatment of inflammatory diseases of the musculoskeletal system, a complex of rehabilitation measures after injury.
- Load restriction, a healthy lifestyle, and proper nutrition are a factor in the fight against overweight.
- Prompt orthopedic correction of skeletal deformities acquired during life.
Remember, it is very important to contact an expert promptly should a problem arise. Late initiation of treatment increases the risk of possible negative consequences of the disease.



















